J Hematol Oncol:BRD4抑制RhoB转录,促进终末红细胞生成
21小时前 吾乃喵大人 MedSci原创 发表于上海
研究揭示BRD4调控细胞增殖的作用则依赖于其与CDK9的经典复合物结合。这一发现不仅丰富了BRD4的功能认知,也为体外血细胞生成及相关疾病的治疗提供了新靶点。
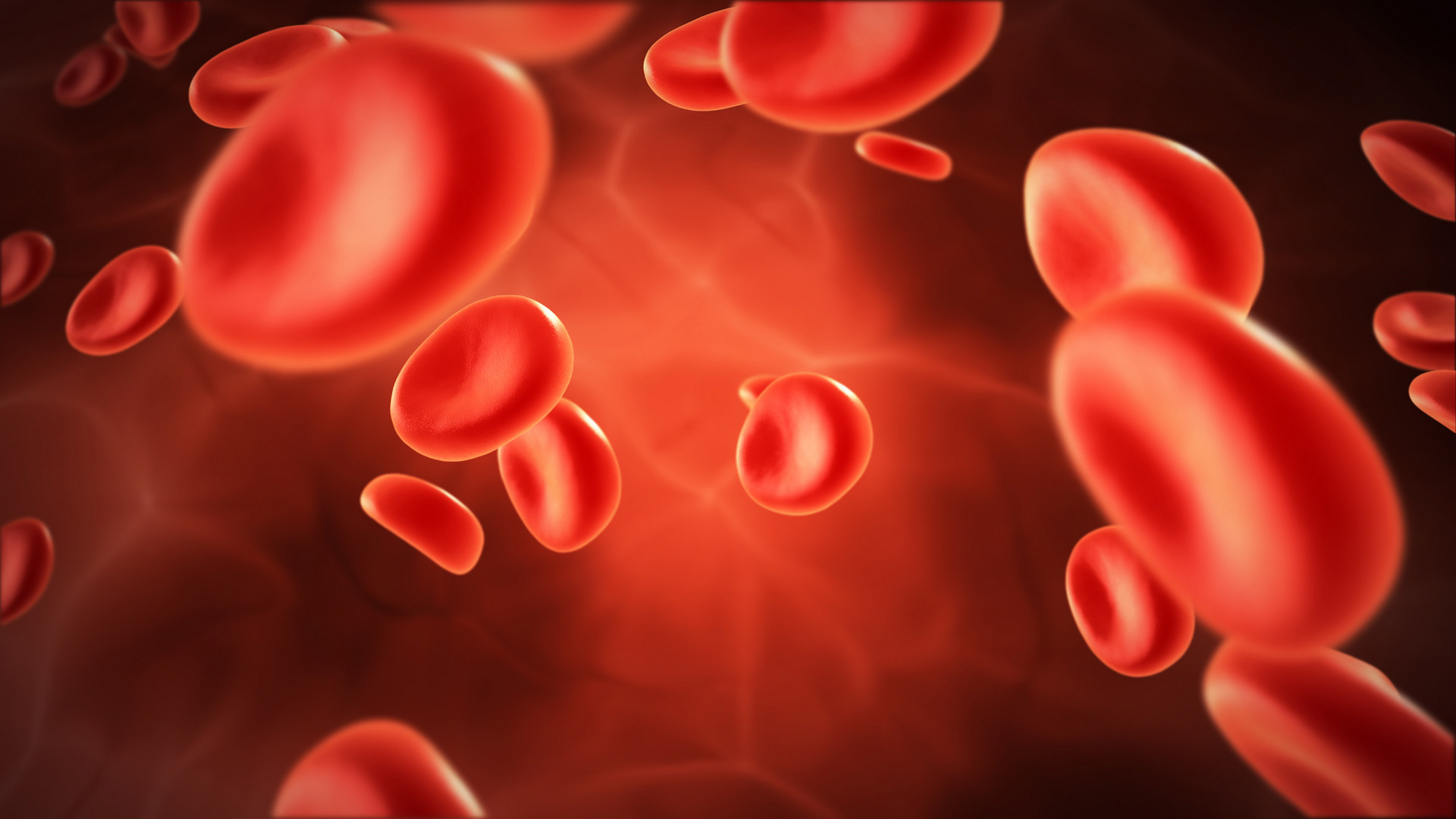
研究亮点 报告发现,表观遗传调控因子BRD4通过抑制RhoB的表达,负向调控人类红细胞终末分化过程。 BRD4促进细胞增殖的经典机制依赖于其CDK9结合功能,而促进红细胞成熟则独立于CDK9,揭示了BRD4的非典型转录抑制功能。 阻断BRD4与组蛋白甲基转移酶EHMT1/2的相互作用解除对RhoB的转录抑制,继而通过调控肌动蛋白重组促进红细胞终末分化和核排出。 红细胞的产生始于造血干/祖细胞(HSCs),经历早期分化、终末分化以及网织红细胞成熟。终末红细胞生成过程中,细胞经历从原红细胞到幼稚红细胞、基底性红细胞、多染性红细胞以及正染性红细胞的连续分化阶段,同时伴有DNA染色质浓缩、细胞及细胞核体积缩小、血红蛋白合成以及膜蛋白重组。精准的转录因子、共激活因子与染色质重塑因子协同,确保红细胞特异性基因的表达正确调控。异常可引发如骨髓增生异常综合征(MDS)、钻石黑芬贫血等病理状态。目前,尽管对于参与终末红细胞分化的转录及表观遗传调控因子已有若干研究,但关键调控因子体系及其作用机制尚不完善。特别,BET家族蛋白中BRD4以其经典结合CDK9促进RNA聚合酶II延伸的激活作用闻名,但其在红细胞
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











前往app查看评论内容
0 0 举报
前往app查看评论内容
0 0 举报
前往app查看评论内容
0 0 举报
前往app查看评论内容
0 0 举报
前往app查看评论内容
0 0 举报
#BRD4# #终末红细胞生成#
3 举报