Thorac Cancer:局部晚期可切除食管鳞状细胞癌(ESCC)使用脂质体紫杉醇+铂类方案作为新辅助化疗的疗效和安全性
2022-02-06 yd2015 MedSci原创
研究表明,脂体紫杉醇联合铂作为新辅助化疗对局部晚期可切除的ESCC患者可提供满意的R0切除率和生存率,且肿瘤降期效果显著,安全可控。
近期,Thoracic Cancer杂志上发表了一项回顾性研究成果,主要是评估局部晚期可切除食管鳞状细胞癌(ESCC)使用脂质体紫杉醇+铂类方案作为新辅助化疗的疗效和安全性。
收集2018年7月至2019年10月接受脂体紫杉醇+铂(顺铂、奈达铂或卡铂)术前新辅助化疗的局部晚期可切除的ESCC患者(分期cT2N + M0, cT3-4aNanyM0, IA-IVA)的资料。本研究的主要终点为R0切除术率,次要终点为病理完全缓解(pCR)率、1年和2年总生存率(OS)率、1年和18个月无病生存率(DFS)率和安全性。
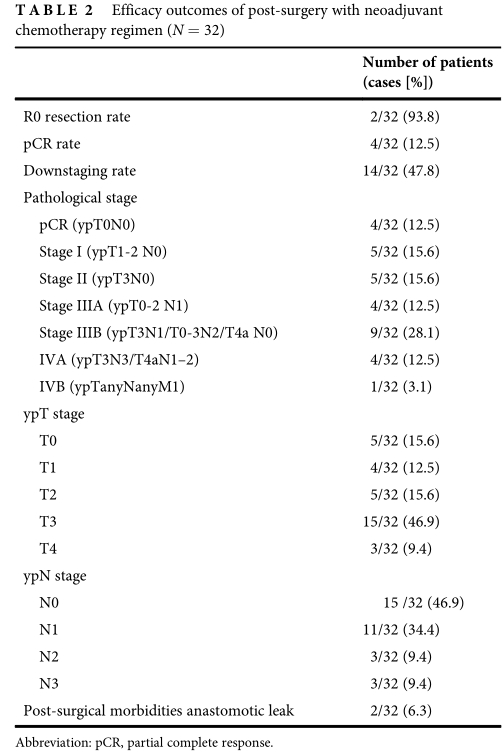
本研究共纳入32例符合条件的患者。所有患者均接受新辅助化疗和手术治疗。中位年龄62.5岁(范围48-71岁),男性26例(81.3%)。T3期有26例(65.6%),T4a占21.9%(7/32),有淋巴结转移22例(68.8%)。组织学分级为G2和G3的患者分别为21例(65.6%)和9例(28.1%),组织学分级未知的患者为2例(6.3%)。II期、III期、IVA期患者分别为10例(31.3%)、15例(46.9%)、7例(21.9%)。
R0切除率为93.8%,pCR率为12.5%,降期率43.8%(14/32),降至I期5例(ypT0 2N0M0), N0期15例(46.9%),淋巴结转移17例(N1期11例,N2期3例,N3期3例)。
疗效评估
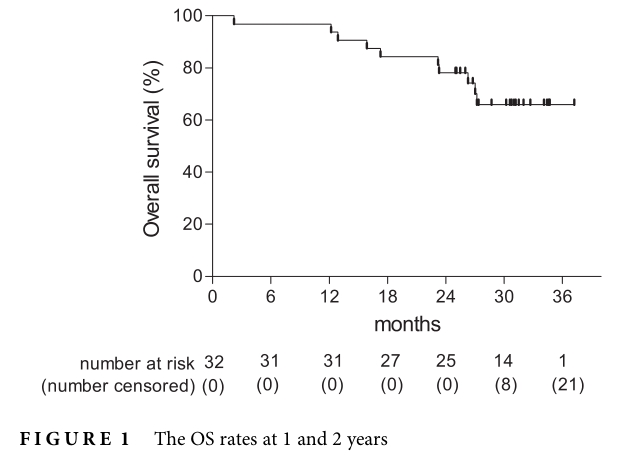
中位随访为31.0个月(95%可信区间[CI] 30.1 - 31.9个月)。1年和2年OS率分别为96.9%和78.1%。中位OS尚未达到。
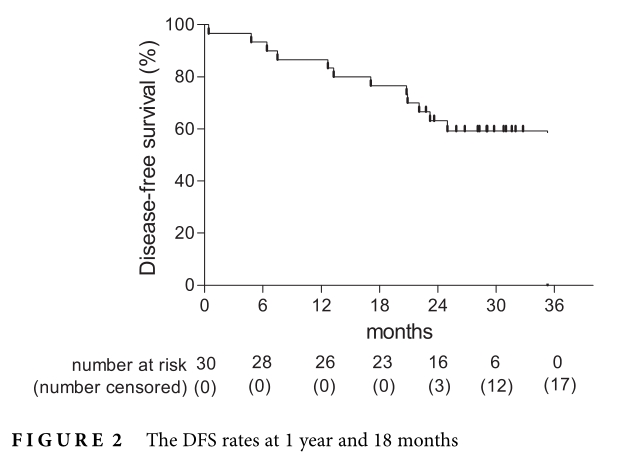
1年和18个月DFS率分别为86.7%和76.7%。中位DFS未达到。
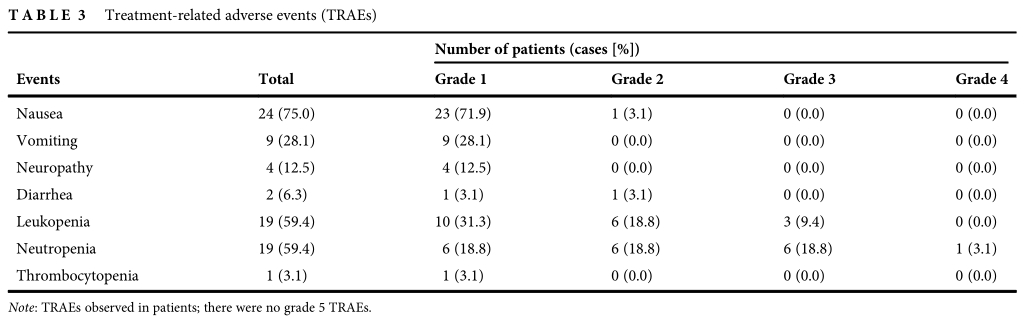
新辅助化疗相关3-4级不良事件发生率为21.9%,其中中性粒细胞减少症(21.9%)、白细胞减少症(9.4%)。无相关死亡病例出现。
综上,研究表明,脂体紫杉醇联合铂作为新辅助化疗对局部晚期可切除的ESCC患者可提供满意的R0切除率和生存率,且肿瘤降期效果显著,安全可控。
原始出处:
Wang W, Yi Y, Jia Y, Dong X, Zhang J, Song X, Song Y. Neoadjuvant chemotherapy with liposomal paclitaxel plus platinum for locally advanced esophageal squamous cell cancer: Results from a retrospective study. Thorac Cancer. 2022 Feb 4. doi: 10.1111/1759-7714.14328. Epub ahead of print. PMID: 35118824.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#THORAC#
119
#脂质体#
105
#铂#
144
#SCC#
89
#细胞癌#
93
#局部晚期#
89
#新辅助#
84
新方法,值得学习
99
#食管鳞状细胞癌#
120
#局部#
104