JAMA Netw Open:种族中性方程助力黑人患者精准诊断肺部疾病
17小时前 刘少飞 MedSci原创 发表于陕西省
这项研究强调了采用种族中性肺功能参考方程对黑人患者进行肺功能评估的重要性,表明在不考虑种族差异的情况下,能够更清晰地揭示肺部病变,避免因种族调整系数带来的偏差。
背景: 在肺功能测试中使用种族调整系数已成为近年来的讨论热点。最近,全球肺功能倡议(GLI)发布了种族中性参考方程(GLI Global),它为不考虑种族背景的肺功能评估提供了新的标准。然而,GLI Global与传统的基于种族的参考方程(GLI 2012)在临床应用中的差异,特别是在肺功能轨迹上的影响尚未得到充分评估。
研究目的: 本研究的目标是比较GLI 2012与GLI Global参考方程在评估肺功能轨迹方面的影响,重点分析两种参考方程对患者肺功能变化的再分类效果,特别是在不同种族群体中的差异。
研究设计与方法: 这项队列研究在麻省总医院进行,分析了1997年1月1日至2020年12月31日期间,年龄在18至95岁之间并完成肺功能检测的患者数据。数据分析工作于2023年1月至2024年11月之间进行。研究团队使用GLI Global和GLI 2012两种参考方程分别计算强制呼气量(FEV1)和强制肺活量(FVC)的z分数,进而评估不同患者群体的肺功能轨迹。
主要结果: 共有24,662名患者参与了本次研究,其中包括988名黑人患者(4.0%)和22,297名白人患者(90.4%)。平均年龄为57.6岁(标准差为15.7岁),其中13,108名为女性(53.2%)。在黑人患者中,190名患者的FEV1或FVC从正常重新分类为异常,这些患者使用GLI Global参考方程后,表现出FEV1的下降(-2.06%),与那些在GLI 2012和GLI Global方程下均被分类为异常的患者(-1.89%)的下降幅度相似。在白人患者中,3348名患者的FEV1或FVC从异常重新分类为正常,这些患者的FEV1下降幅度(-1.82%)与正常肺功能的患者(-1.97%)无显著差异,不论使用哪种参考方程。
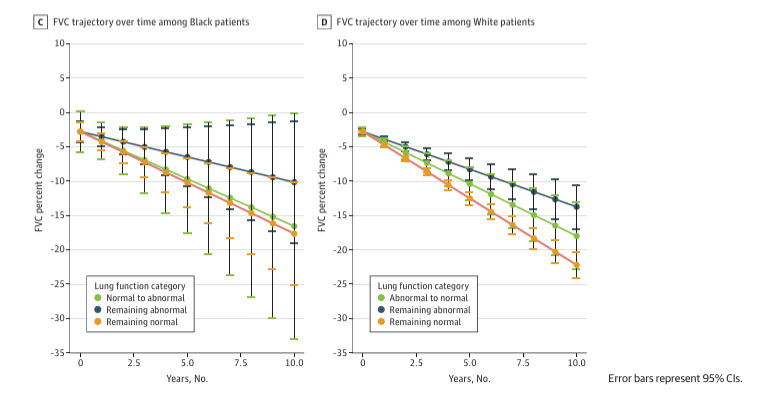
研究结论与意义: 本研究发现,使用种族中性参考方程GLI Global重新分类为异常的黑人患者,其FEV1下降幅度与那些在GLI 2012和GLI Global方程下均被分类为异常的患者相似。这一发现表明,种族中性的肺功能解读方式可能为黑人患者提供更准确的肺部病变识别,尤其在避免过度依赖种族调整系数的情况下,有助于更准确地诊断肺部疾病的进展。
总结: 这项研究强调了采用种族中性肺功能参考方程对黑人患者进行肺功能评估的重要性,表明在不考虑种族差异的情况下,能够更清晰地揭示肺部病变,避免因种族调整系数带来的偏差。这一发现为今后在不同人群中应用肺功能测试提供了新的视角,具有重要的临床意义。
参考文献:
Vyas DA, Zhao S, Lai PS, Rodriguez-Lopez J, Schmidt EP, Brown R, Hibbert KA, Hardin CC, North CM. Lung Function Trajectory Using Race-Specific vs Race-Neutral Global Lung Function Initiative Coefficients. JAMA Netw Open. 2025 Apr 1;8(4):e257304. doi: 10.1001/jamanetworkopen.2025.7304. PMID: 40279124; PMCID: PMC12032560.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















前往app查看评论内容
0 0
前往app查看评论内容
4 0
前往app查看评论内容
4 0
前往app查看评论内容
0 0
前往app查看评论内容
6 0
前往app查看评论内容
8 0