BTK抑制剂tolebrutinib治疗多发性硬化症 (MS) ,显示出“有希望”的结果
2021-10-14 Allan MedSci原创
多发性硬化症(MS)是一种脱髓鞘性神经病变,患者脑或脊髓中的神经细胞表面的绝缘物质(即髓鞘)受到破坏,神经系统的信号转导受损,导致一系列可能发生的症状,影响患者的活动、心智、甚至精神状态。
多发性硬化症(MS)是一种脱髓鞘性神经病变,患者脑或脊髓中的神经细胞表面的绝缘物质(即髓鞘)受到破坏,神经系统的信号转导受损,导致一系列可能发生的症状,影响患者的活动、心智、甚至精神状态。这些症状可能包括复视、单侧视力受损、肌肉无力、感觉迟钝,或协调障碍。多发性硬化症的病情多变,患者的症状可能反复发作,也可能持续加剧。
多发性硬化症发生的三个重要特征包含出现中枢神经系统病灶、发炎反应,以及髓鞘破坏等。本疾病最常进犯视神经、脑干、基底核、脊髓,以及侧脑室周围的白质。
近日,法国制药公司赛诺菲公布了其研究性口服布鲁顿酪氨酸激酶 (BTK) 抑制剂tolebrutinib的新长期数据,结果显示,tolebrutinib在复发难治多发性硬化症 (MS) 患者中显示出“有希望的”安全性和有效性。
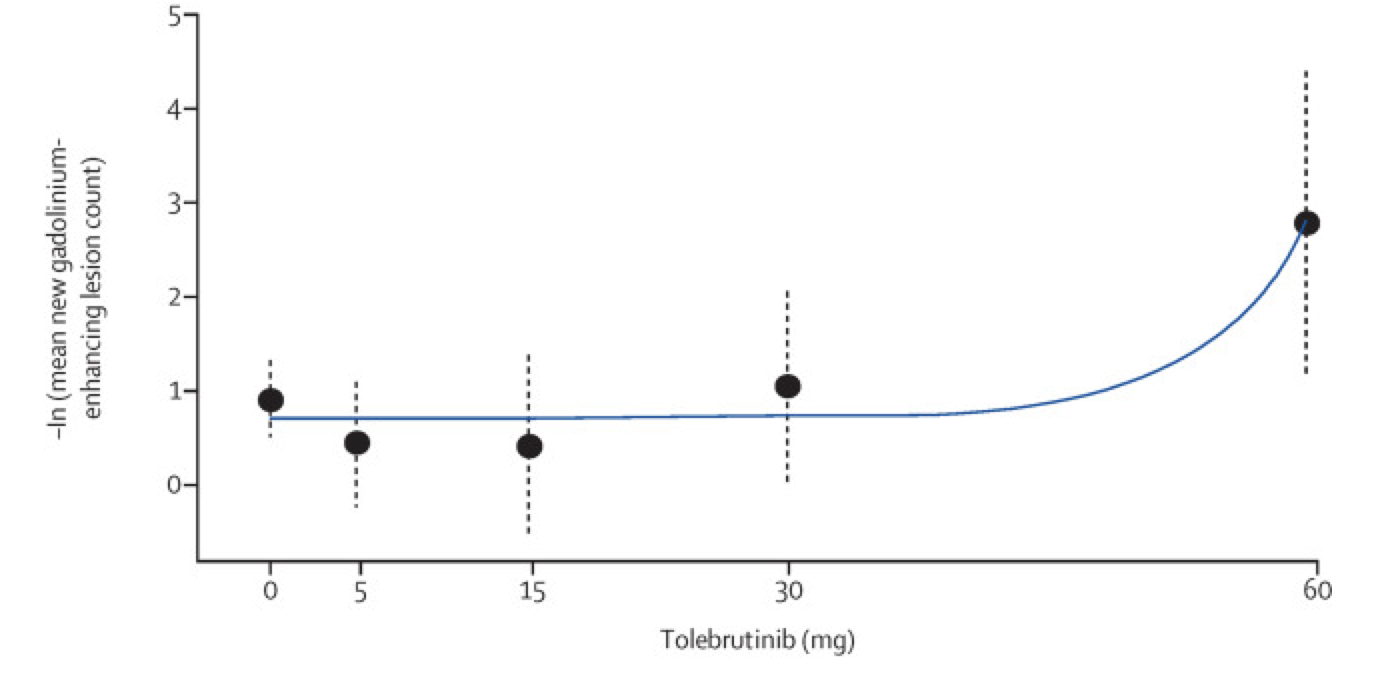
图1. 应用两步多重比较程序和建模后的估计剂量反应曲线
IIb期长期扩展研究 (LTS) 的结果表明,在治疗48周后,BTK抑制剂tolebrutinib降低了多发性硬化症 (MS) 疾病的活动度。
据赛诺菲称,根据“公开信息”,该数据使tolebrutinib成为唯一一种正在开发的用于MS的BTK抑制剂,该抑制剂已被证明可以直接调节小胶质细胞。
赛诺菲神经病学开发领域负责人Erik Wallström说:“了解脑渗透疗法减缓残疾积累的能力,有可能为难治性MS患者带来新的希望。近二十年来,赛诺菲一直坚定不移地努力加快为这些患者提供治疗方案”。
目前,tolebrutinib正在III期临床试验中进行评估,用于治疗MS、非复发性继发性进展性MS (nrSPMS) 和原发性进展性 MS (PPMS)。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#多发性#
92 举报
#硬化症#
98 举报
#抑制剂#
125 举报
#BTK抑制剂#
128 举报
#BTK#
99 举报